Digestive symptoms like abdominal pain, bloating, and changes in bowel habits are common complaints that often point to conditions like Irritable Bowel Syndrome (IBS) or Inflammatory Bowel Disease (IBD). However, in some cases, they may be signs of something more serious, such as colorectal cancer.
Distinguishing between these conditions can be challenging because they share many overlapping symptoms. Understanding the differences, especially when it comes to colon cancer warning signs, can help patients and healthcare providers make more informed decisions about testing, diagnosis, and treatment.
Shared Symptoms: Why Confusion Happens
IBS, IBD, and colon cancer all affect the gastrointestinal tract, and many of the early symptoms of colon cancer look similar. These include:
- Abdominal discomfort or cramping
- Bloating or gas
- Diarrhea or constipation
- Changes in stool appearance or frequency
- Urgency or incomplete evacuation
Because these symptoms can range from mild to severe and fluctuate over time, many people dismiss them as temporary or diet-related issues. This overlap is a major reason why colon cancer may go undetected until later stages if not properly evaluated.
The key difference lies in the persistence, progression, and combination of symptoms. That’s why it’s essential to monitor changes and speak to a healthcare provider when symptoms don’t improve.
IBS: A Functional but Non-Inflammatory Condition
Irritable Bowel Syndrome is a chronic disorder that affects how the muscles in the bowel contract and how the brain communicates with the gut. It’s considered a functional condition, meaning there’s no visible damage or inflammation to the intestines.
IBS typically causes:
- Abdominal pain relieved by bowel movements
- Bloating
- Alternating constipation and diarrhea
- Mucus in the stool
Importantly, IBS does not cause weight loss, rectal bleeding, or long-term damage to the intestines. While it can significantly impact quality of life, it does not raise the risk of colon cancer or progress into a more serious condition. Diagnosis is made based on symptom history and by ruling out other conditions. Colonoscopy and lab tests are often normal in people with IBS.
IBD: A Chronic Inflammatory Disease
Inflammatory Bowel Disease, which includes Crohn’s disease and ulcerative colitis, involves ongoing inflammation of the digestive tract. Unlike IBS, IBD causes physical damage to the lining of the intestines, which can be seen during imaging or endoscopy.
Common symptoms include:
- Bloody diarrhea
- Ongoing abdominal pain
- Fatigue and fever
- Weight loss
- Anemia
IBD can come and go in flares, with periods of remission in between. Over time, chronic inflammation can lead to complications like strictures, fistulas, and even an increased risk of colorectal cancer. That’s why people with IBD are advised to undergo regular screening colonoscopies starting earlier than the general population.
Colon Cancer Symptoms: What Sets Them Apart
Colorectal cancer often begins silently, with symptoms that mimic IBS or IBD. However, there are specific colon cancer symptoms that warrant closer attention:
- Rectal bleeding or blood in the stool
- Unexplained weight loss
- Persistent changes in bowel habits
- Feeling that the bowel doesn’t empty completely
- Fatigue caused by anemia
- Narrow or ribbon-like stools
These symptoms tend to worsen over time and do not respond to dietary changes or standard treatments for IBS or IBD. Blood in the stool, especially if it’s dark or mixed into the stool, should always be evaluated promptly.
The presence of more than one of these warning signs, especially in people over 45 or those with a family history, should prompt further testing, including colonoscopy.
Diagnosis: How Doctors Tell Them Apart
To determine whether symptoms are caused by IBS, IBD, or something more serious like colorectal cancer, doctors use a combination of medical history, physical exams, and diagnostic tests.
These may include:
- Blood tests to check for anemia or signs of inflammation
- Stool tests to rule out infections or detect hidden blood
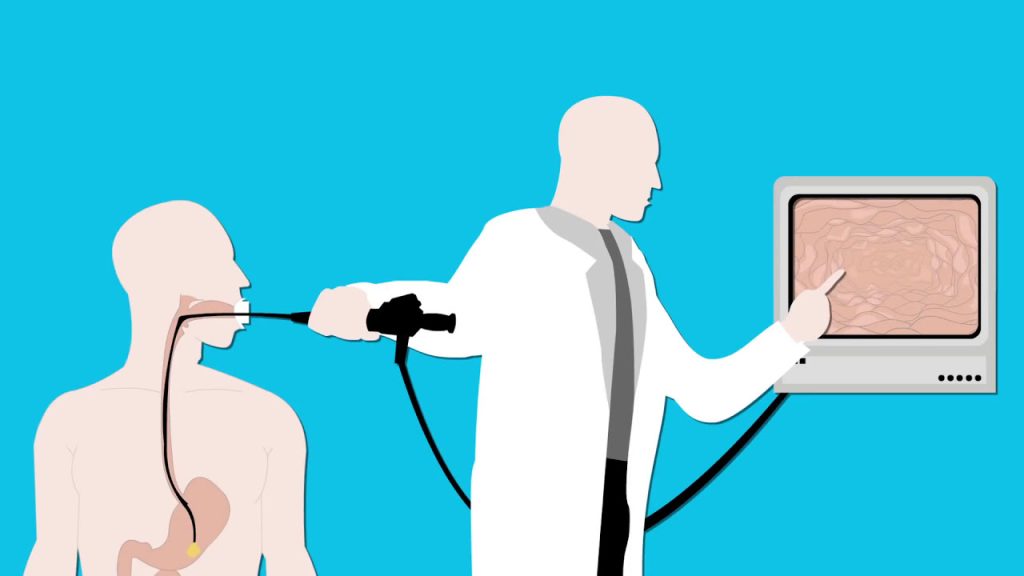
- Colonoscopy to directly view the colon lining and take biopsies
- Imaging studies like CT scans or MRIs
A colonoscopy remains the gold standard for diagnosing colon cancer symptoms, identifying polyps, and determining whether there’s inflammation or visible disease.
When to Seek Medical Advice
While occasional digestive issues are normal, symptoms that persist for more than a few weeks should never be ignored. Anyone experiencing rectal bleeding, unexplained weight loss, or ongoing changes in bowel habits should see a healthcare provider as soon as possible.
Even if the cause turns out to be IBS or IBD, early diagnosis can lead to more effective symptom management. And if cancer is suspected, early detection dramatically improves treatment outcomes.
Conclusion
IBS, IBD, and colon cancer can all cause digestive discomfort, but their underlying causes and long-term risks are very different. Paying attention to the nature, frequency, and progression of symptoms is crucial.
While many people may assume their issues are minor, it’s important not to overlook potential colon cancer symptoms, especially when they persist or worsen. If you’re unsure about your symptoms, don’t delay seeking medical advice. In many cases, timely diagnosis can not only improve quality of life—but save it.

Comments are closed.